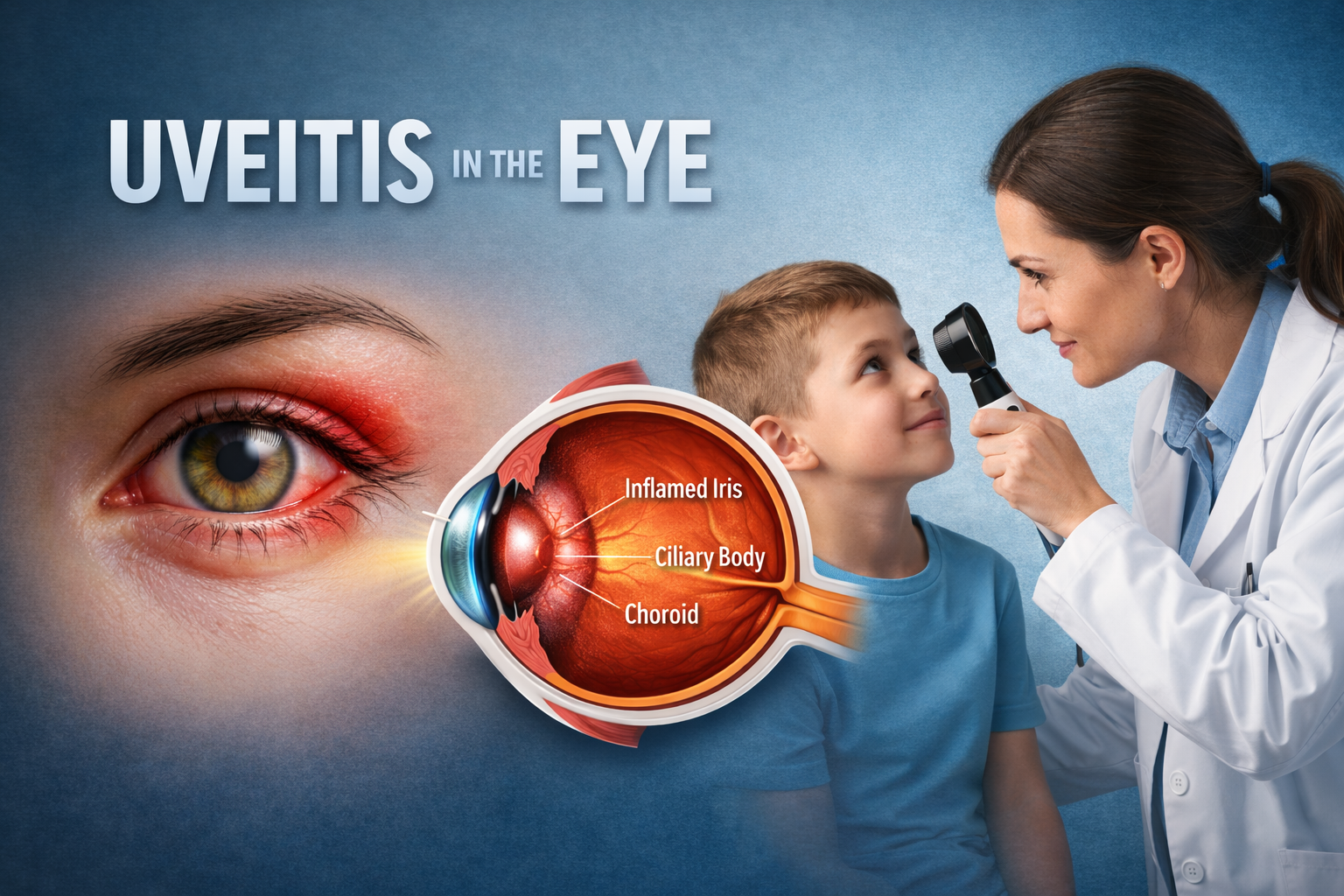
Uveitis in Eye: Types, Symptoms and Treatment
The human eye is a sensitive organ, and a slight inflammation of the organ can greatly disturb vision. Uveitis is one such disorder that is a potentially serious inflammation of the uvea, the layer of tissue containing the iris, ciliary body, and the choroid. Patients tend to first ask, what is uveitis, and how can it damage their vision. Uveitis can present itself suddenly, but can also develop with time, with a range of influences from mild discomfort to a severe threat with permanent damage.
Knowing uveitis symptoms, causes, and treatment options is of great value to avoid unnecessary delays in receiving proper medical attention. This condition can also present itself with systemic diseases, so a uveitis specialist/neuro ophthalmologist is needed. This is to address the types of uveitis, their warning signs, complications, and the most effective means of addressing this condition, uveitis.
|
Content of The Article |
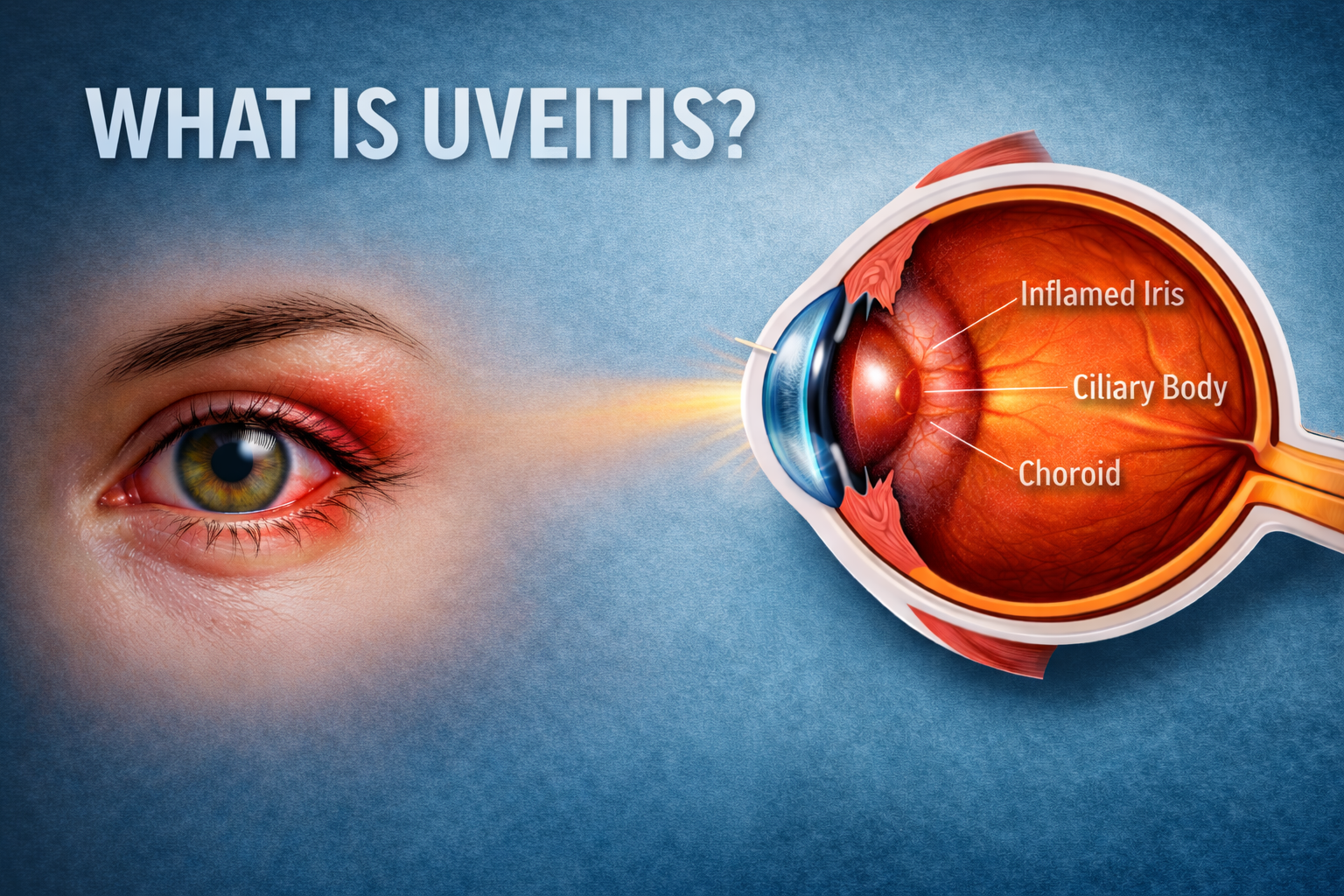
What is Uveitis?
Uveitis is also called inflammation of the uvea, which is the middle layer of the eye and is responsible for nourishing crucial components like the retina. The uvea is subdivided into three sections:
- The iris (anterior layer).
- The ciliary body (middle layer).
- The choroid (posterior layer).
Uveitis is an inflammation that can affect any of these parts and is often due to an injury to the eye, autoimmune disorders, and infections. The inflammation usually starts in one region, but can quickly move to and affect the other components and the overall health of the eye. Uveitis can result in inflammation of and subsequent injury to other internal, vital structures such as the retina and optic nerve, so it should never be neglected.
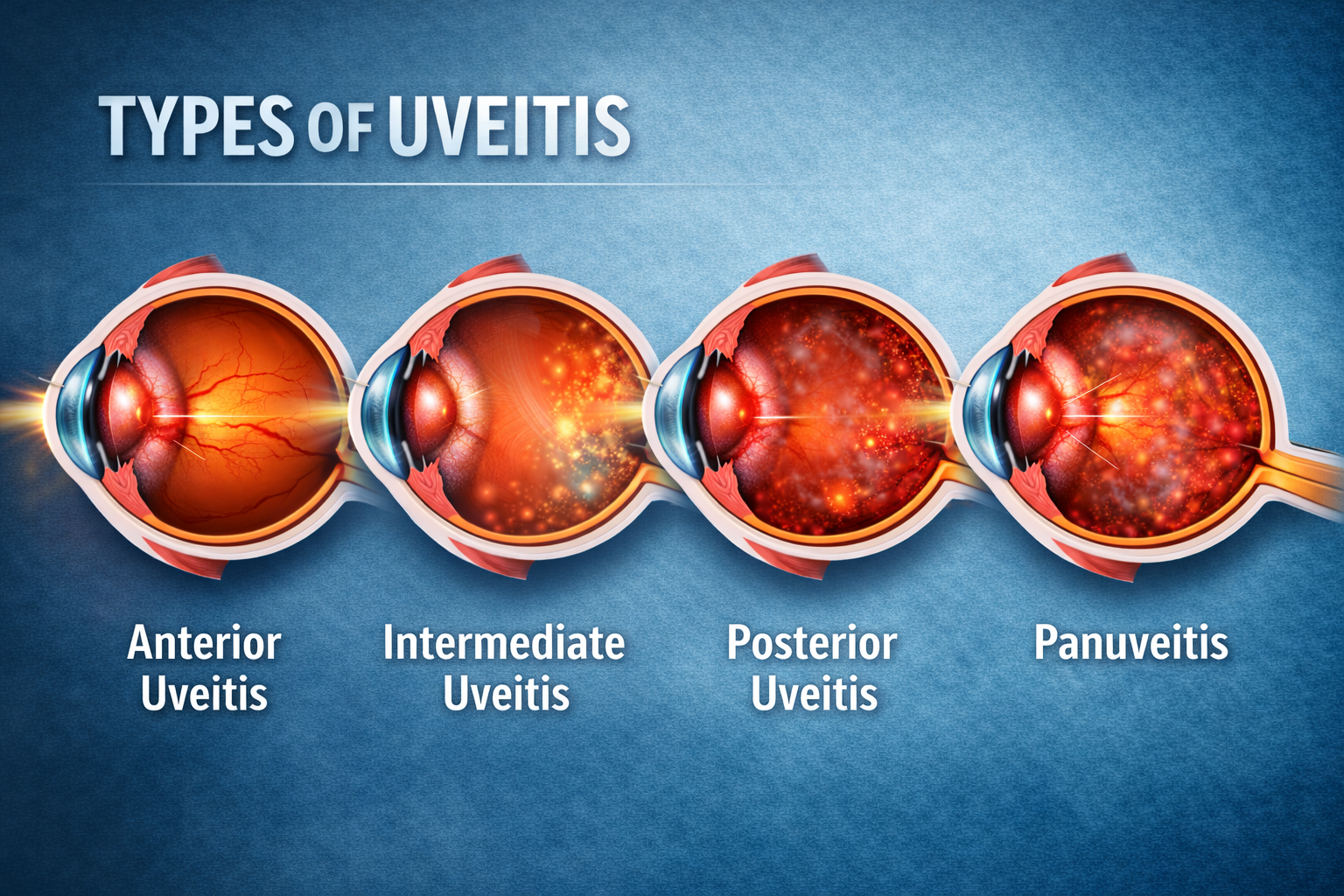
Types of Uveitis
Uveitis is usually classified according to the inflamed uvea region. This classification is relevant for uveitis patients since it directly correlates to the potential level of risk and the corresponding treatment possibilities.
1. Anterior Uveitis
This type is the most prevalent and impacts the anterior region of the eye. This type is also referred to as iritis. The most common symptoms of this disease include pain, marginal inflammation, and photophobia.
2. Intermediate Uveitis
This occurs in the vitreous body of the eye, which is the gel mass that occupies the eye’s centre. During this type of uveitis, patients may experience the occurrence of floaters, and vision may become obscured.
3. Posterior Uveitis
This form affects the back of the eye, more specifically, the choroid and retina. Due to the serious and permanent vision loss that can stem from this form, it remains one of the most concerning types of uveitis.
4. Panuveitis
This type presents with inflammation of all sections of the uvea. Panuveitis, and all of its forms, can involve severe manifestations and have a notable association with autoimmune and infectious diseases.
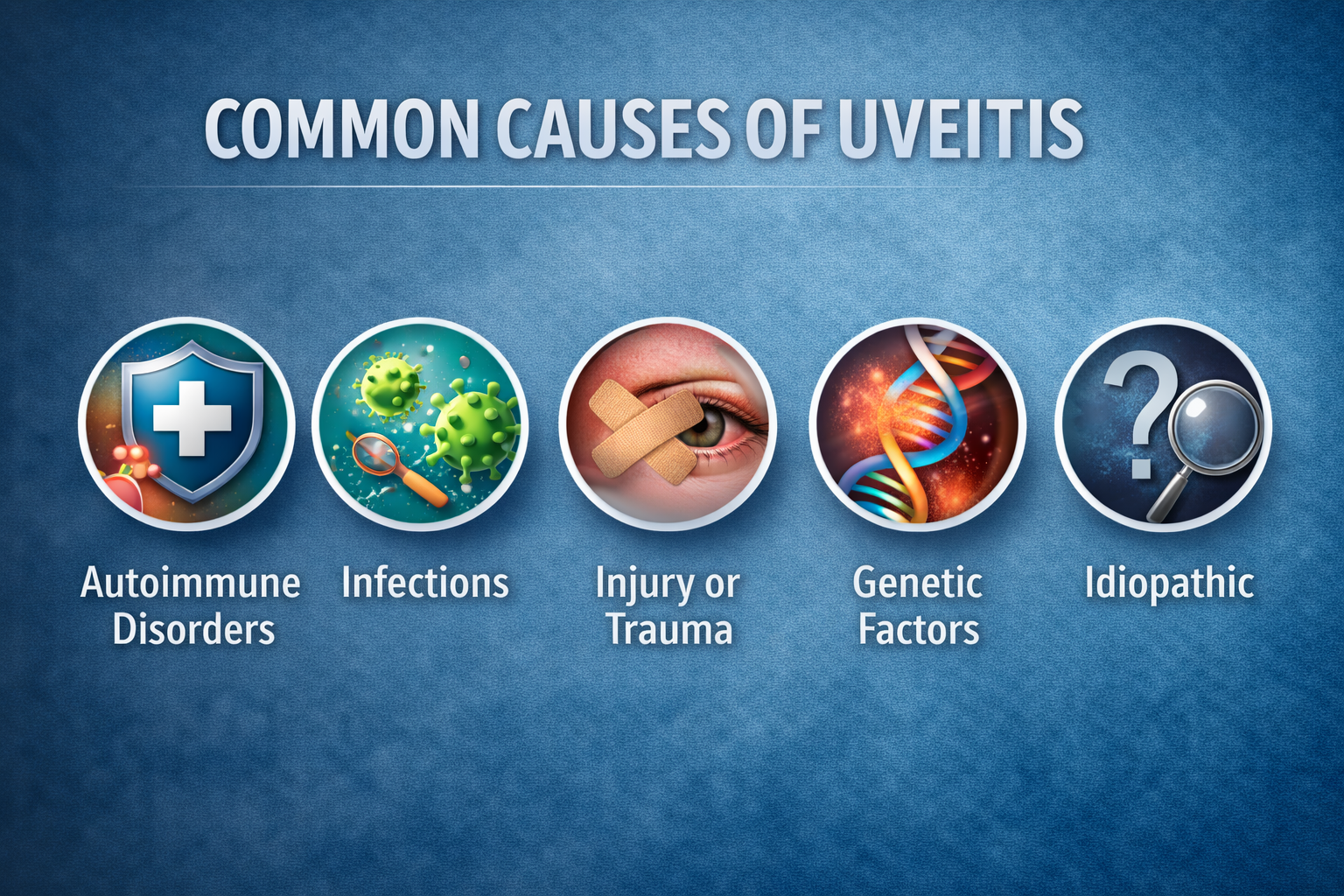
Common Causes of Uveitis
Examine the descriptive features of uveitis and its potential causes, and you will note that it has a very distinct, elusive, and yet harmonious beauty likely due to the existence of its many multifaceted potential causes. The most common of these causes are:
Autoimmune Disorders
Several disorders characterised by inflammation of the eyes include rheumatoid arthritis, lupus, ankylosing spondylitis, and sarcoidosis. These conditions trigger abnormal immune responses, causing the body to attack healthy ocular tissues, leading to recurrent or chronic inflammation that may affect vision if not adequately managed. These infections can directly invade ocular tissues or provoke immune-mediated inflammation, making early diagnosis and appropriate antimicrobial treatment essential to prevent complications and long-term visual impairment.
Infections
Many bacterial (TB, syphilis), certain viral (e.g., herpes), fungal and parasitic infections may contribute to the development of uveitis. These infections can directly invade ocular tissues or provoke immune-mediated inflammation, making early diagnosis and appropriate antimicrobial treatment essential to prevent complications and long-term visual impairment.
Injury or Trauma
The uveal tissues of the eye may become inflamed by a blunt or penetrating injury. Trauma can disrupt the eye’s protective barriers, triggering inflammation or allowing infectious agents to enter, which may result in acute uveitis or delayed inflammatory responses.
Genetic Factors
Higher risk groups may carry certain genetic markers such as HLA-B27. Individuals with these genetic predispositions are more prone to recurrent or severe uveitis, often associated with systemic inflammatory conditions, highlighting the role of genetics in disease susceptibility.
Unknown (Idiopathic)
in up to 50% of people, this and many other triggers of uveitis cannot be fully elucidated. Despite extensive evaluation, no identifiable cause is found, suggesting complex immune mechanisms or unidentified environmental factors may play a role in disease development.
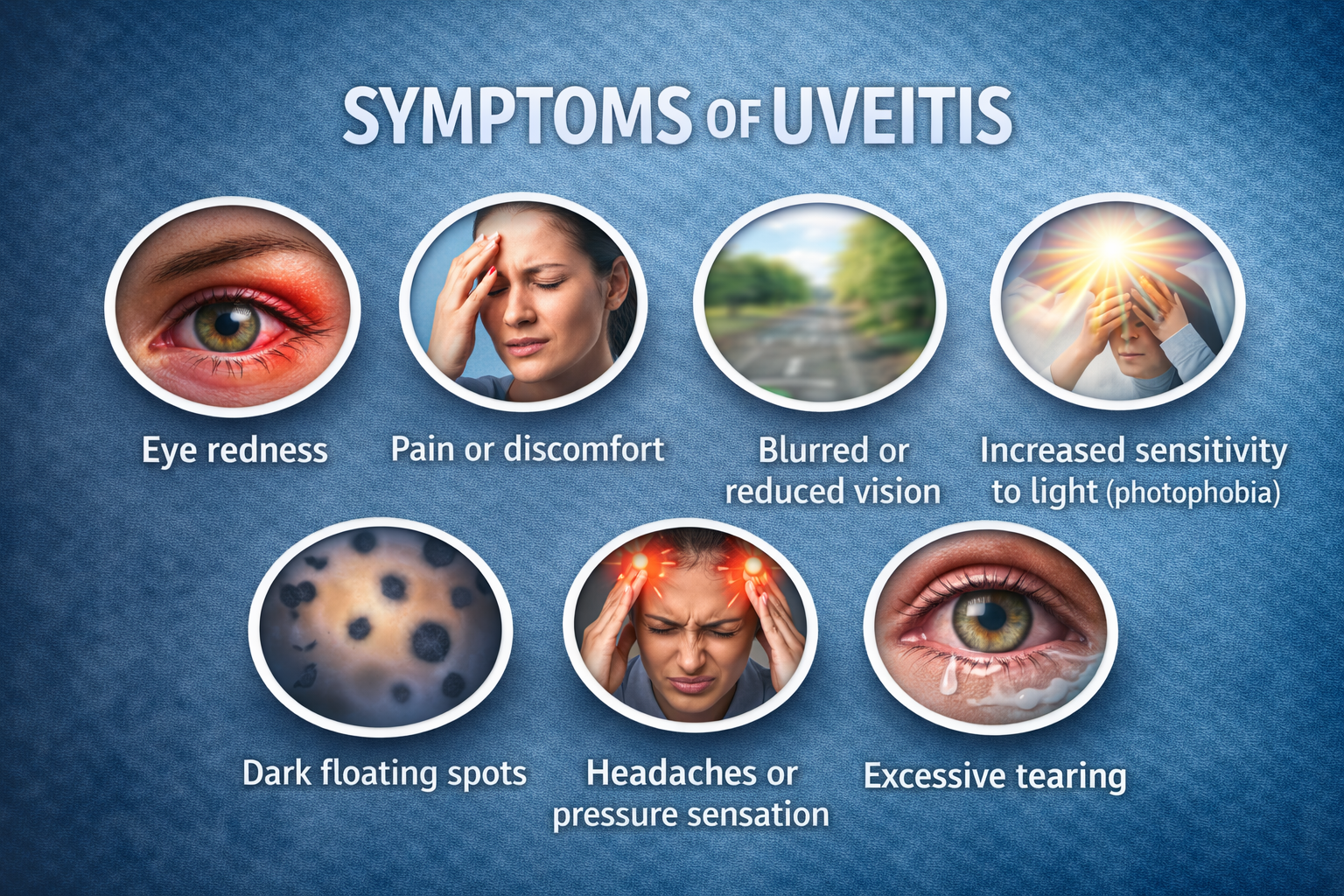
Uveitis Symptoms You Should Know
It is important to recognise the key uveitis symptoms early, as the condition is uveitis symptoms such as:
- Eye redness: Eye redness occurs when the small blood vessels on the surface of the eye become dilated or irritated. This may result from infection, inflammation, dryness, allergy, or strain. Redness often signals an underlying eye condition that may require rest, lubrication, or medical evaluation if persistent.
- Pain or discomfort: Eye pain or discomfort can range from mild irritation to sharp or aching pain. It may be caused by dryness, infection, inflammation, foreign bodies, or increased eye pressure. Persistent pain should not be ignored, as it can indicate serious conditions affecting the cornea or internal eye structures.
- Increased sensitivity to light (photophobia): Photophobia is an abnormal sensitivity to light that causes discomfort or pain when exposed to bright environments. It often occurs with eye inflammation, infections, migraines, or corneal problems. This symptom suggests irritation of light-sensitive structures and may significantly interfere with daily activities.
- Blurred or reduced vision: Blurred or reduced vision means a loss of sharpness or clarity in seeing objects. It may result from refractive errors, inflammation, infection, swelling, or damage to the retina or optic nerve. Sudden or worsening vision changes are concerning and should be evaluated promptly.
- Dark floating spots: Dark floating spots, also known as floaters, appear as moving dots, threads, or shadows in the field of vision. They are caused by tiny particles or changes within the vitreous gel of the eye. While often harmless, a sudden increase may indicate retinal problems.
- Headaches or pressure sensation: Some individuals experience headaches or a feeling of pressure around or behind the eyes. This can be linked to eye strain, inflammation, or increased intraocular pressure associated with certain types of uveitis.
- Excessive tearing: The eyes may water excessively as a protective response to irritation and inflammation. Although tearing is meant to soothe the eye, constant watering can indicate ongoing inflammation and discomfort requiring medical attention.
Symptoms may appear suddenly (acute uveitis) or gradually (chronic uveitis). If you notice any of these uveitis eye symptoms, pursue medical attention at once.
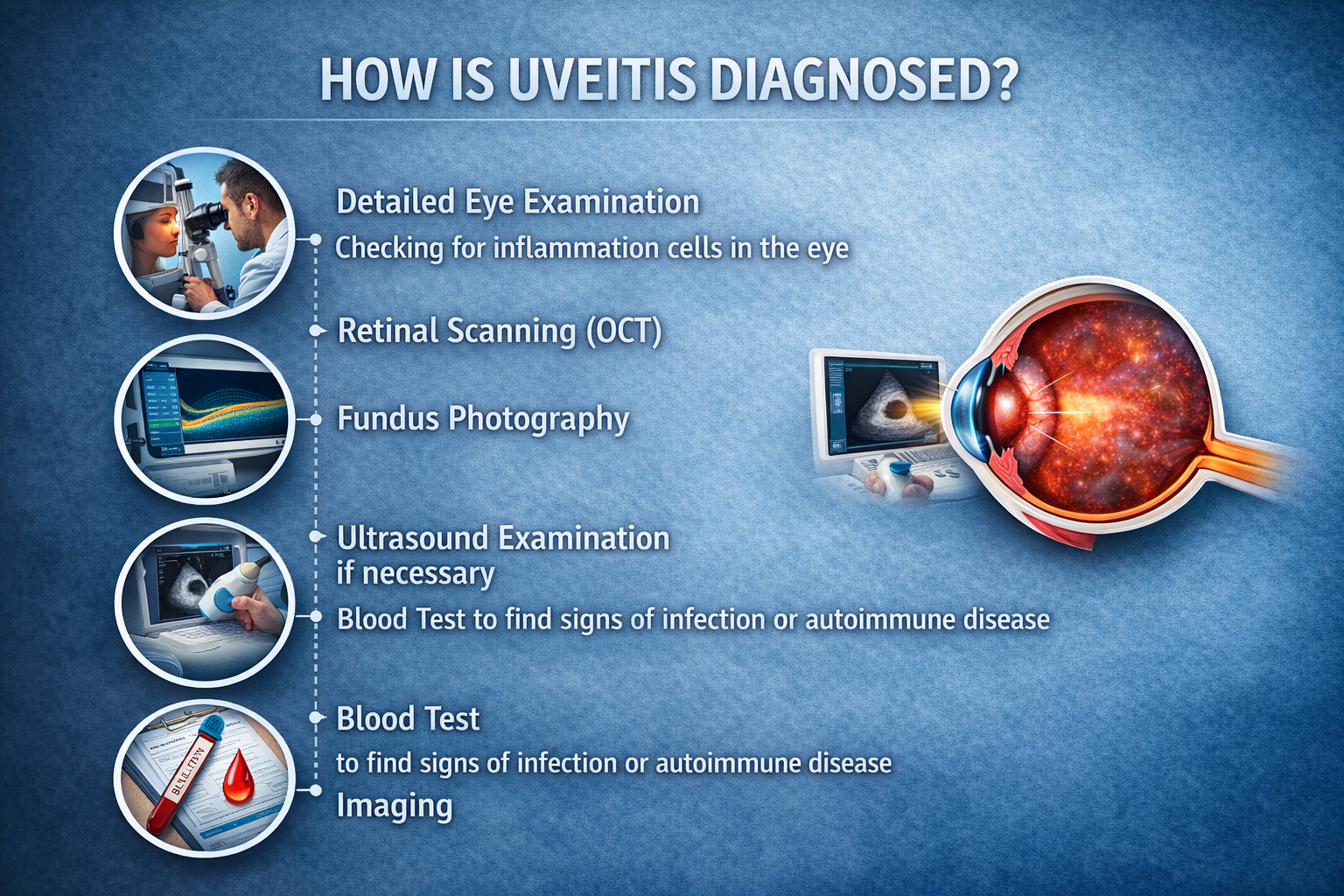
How is Uveitis Diagnosed
A uveitis diagnosis is made following a thorough examination to check iridocyclitis, uveitis, or neuro-ophthalmic eye doctor due to the condition being associated with other systemic diseases. Such examination includes, but is not limited to:
- Detailed eye examination
- Checking for inflammation cells in the eye
- Retinal scanning (OCT)
- Fundus photography
- Ultrasound examination if necessary
- Blood test to find signs of infection or autoimmune disease
- Imaging X-ray or MRI when indicated
Having an early diagnosis is key to preventing long-term complications or serious consequences from arising from uveitis.
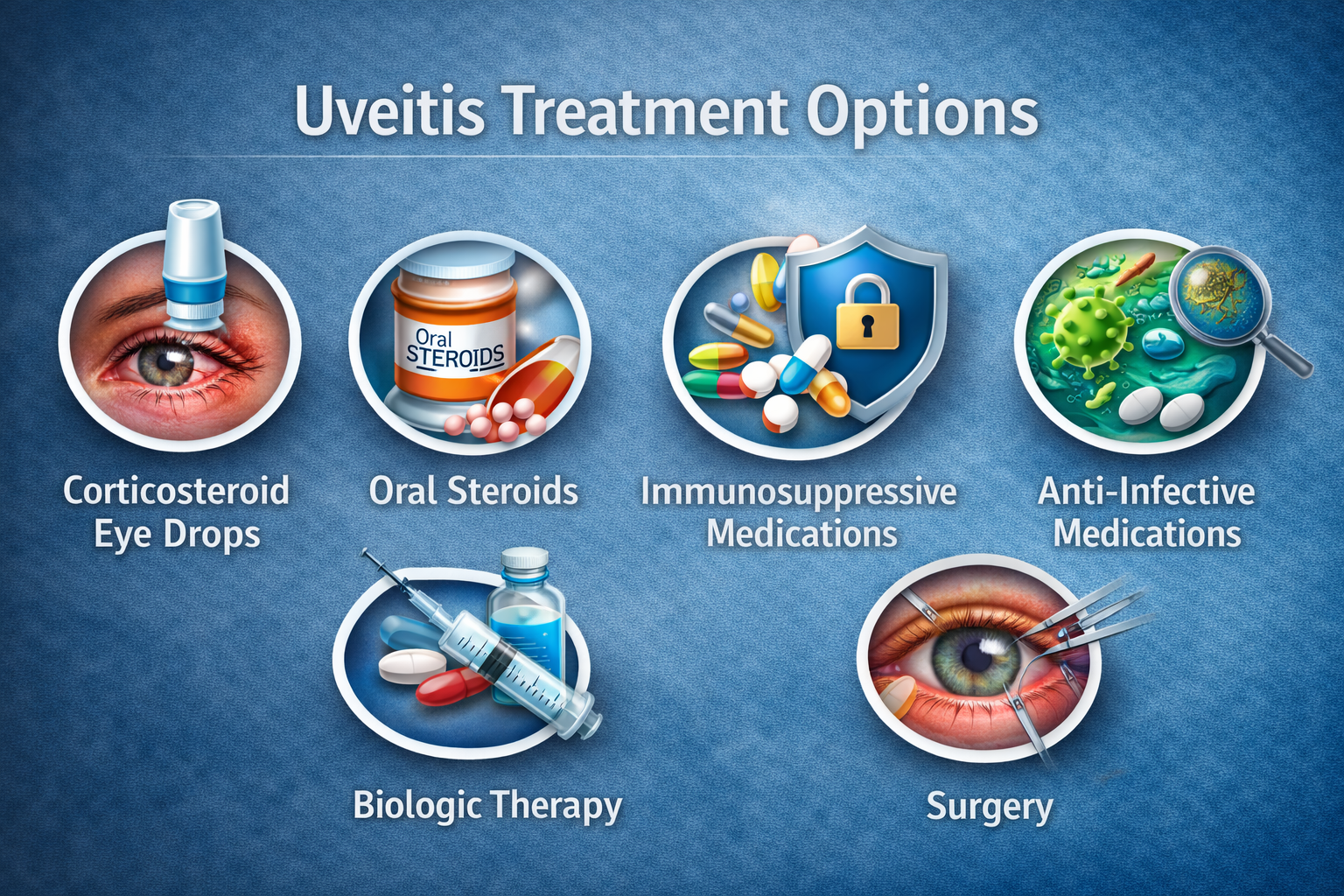
Uveitis Treatment Options
In order to be effective, uveitis treatment have to be based on the type of uveitis, its severity, and the cause if it is known. The goal to achieving this is to alleviate any serious consequences and symptoms that arise from inflammation.
1. Corticosteroid Eye drops
For uveitis treatment, anterior uveitis is prescribed to decrease inflammation. These drops help reduce redness, pain, and light sensitivity, and are usually given frequently at first, then gradually tapered under ophthalmologist supervision to prevent side effects.
2. Oral Steroids
Prescribed when the inflammation is more extensive or more serious. They are useful for bilateral disease or posterior involvement, providing systemic control of inflammation while requiring careful monitoring for long-term adverse effects.
3. Immunosuppressive Medications
Used when the uveitis is associated with autoimmune disorders. These medications help control chronic inflammation, reduce steroid dependence, and are commonly used in conditions like Behçet disease, sarcoidosis, or juvenile idiopathic arthritis.
4. Anti-Infective Medications
Used in the presence of infections: antibiotics, antivirals, or antifungals. Treatment is tailored to the identified organism, ensuring the underlying infection is eliminated while preventing further ocular damage and preserving visual function.
5. Biologic Therapy
In the case of severe or frequent ones, advanced biologic treatments may be necessary. These targeted therapies act on specific immune pathways and are especially helpful in refractory uveitis cases not responding to conventional immunosuppressive drugs.
6. Surgery
In complicated cases, particularly intermediate or posterior uveitis, a vitrectomy may be advised. Surgical intervention can help remove inflammatory debris, improve vision, and manage complications such as retinal detachment or persistent vitreous opacities.
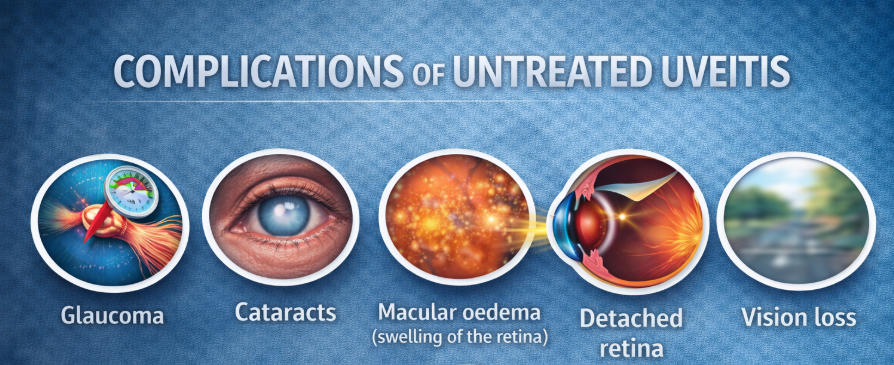
Complications of Untreated Uveitis
Uveitis can lead to severe and irreversible damage if left untreated. Uveitis can lead to the following major complications:
- Glaucoma: Persistent inflammation can raise intraocular pressure, damaging the optic nerve. This may lead to irreversible vision loss if glaucoma is not detected and treated early.
- Cataracts: Chronic uveitis or prolonged steroid use can cause clouding of the eye’s natural lens, resulting in blurred vision and increased sensitivity to light.
- Macular oedema (swelling of the retina): Inflammation may cause fluid accumulation in the macula, the central part of the retina, leading to distorted or reduced central vision
- Detached retina: Severe or longstanding uveitis can weaken retinal structures, increasing the risk of retinal tears or detachment, a sight-threatening emergency.
- Vision loss: Delayed or inadequate treatment may result in cumulative eye damage, scarring, and progressive loss of vision, potentially leading to partial or complete blindness.
Complications can be serious, so prompt consultation with a uveitis specialist is a must.
Tips for Coping with Uveitis
- Take your medications as prescribed.
- Wear sunglasses to block UV light.
- Don’t smoke, as it worsens inflammation.
- Maintain cleanliness to avoid infections.
- Take charge of your autoimmune disorders.
- Don’t forget to go to your follow-up appointments.
Noble Eye Care – Specialist Uveitis Care in India
Complex inflammatory eye disorders like uveitis require expert and thoughtful clinical guidance. Noble Eye Care has built a reputation for excellence in offering complex diagnoses and care for uveitis eye disorders. Their team of ophthalmologists and a neuro ophthalmologist are recognized in their fields for overseeing complex uveitis care. With meticulous planning aligned with advanced imaging and lab resources, it is a clinic that truly takes a tailored approach to patient care.
Noble Eye Care combines precise diagnoses with active chronic disease and complication care. If it is autoimmune uveitis, inflammation due to an infection, or chronic recurrent issues, Noble Eye Care is a uveitis and eye care clinic that understands the importance of clear and advanced approaches to vision preservation.
Also Read: What Is Squint (Strabismus)? Causes, Symptoms, and Treatment
Conclusion
Uveitis can be life-changing, which is why it is important to understand how to recognise its signs and how to seek treatment as early as possible in order to limit the damage to one’s eyesight. Identifying the condition early, whether it stems from infections, autoimmune disorders,/or injuries, can save one’s eyesight. Since the condition can often be linked to larger, more systemic problems, it is vital to consult a uveitis specialist or neuro-ophthalmologist to get the most thorough review of your case.
Most uveitis patients can keep their vision intact with the right help, which can be found at Noble Eye Care, allowing for the care to be tailored to one’s condition.
FAQs About Eye Uveitis
Yes, uveitis can cause permanent vision loss if it is not diagnosed and treated early. Ongoing inflammation may damage important eye structures, leading to complications such as cataracts, glaucoma, retinal damage, or optic nerve injury. Prompt treatment greatly reduces this risk.
Uveitis affects the uvea, the middle layer of the eye, which includes:
- Iris (front of the eye)
- Ciliary body (controls lens focus)
- Choroid (supplies blood to the retina)
Depending on the type, uveitis can also involve the retina, vitreous, or optic nerve.
Doctors may perform:
- Slit-lamp examination to detect inflammation
- Dilated eye exam to assess the retina
- Intraocular pressure testing (to check for glaucoma)
- Blood tests to identify infections or autoimmune diseases
Imaging tests such as OCT, fluorescein angiography, or ultrasound when needed
Uveitis recovery depends on severity and type. Mild anterior uveitis improves within two to six weeks, while posterior or chronic uveitis may require months of treatment and monitoring.
Uveitis may temporarily affect reading or phone use due to blurred vision, eye pain, and light sensitivity. These symptoms usually improve as inflammation reduces with proper treatment.
Follow-up visits are usually frequent initially, often every one to two weeks. As uveitis improves, visits become less frequent, with long-term monitoring for chronic cases.
Uveitis affects the inner eye and can threaten vision, causing pain and blurred sight. Conjunctivitis affects the eye surface, causing redness and discharge, and is usually mild.

Leave a Comment
(0 Comments)